A recent study from Sweden has investigated how antidepressants affect dementia, fracture risk and mortality. The results are alarming: there is a significant link between taking antidepressants and a worsening of dementia, an increased risk of bone fractures and a higher mortality rate.
Antidepressants and their risks
The study shows that selective serotonin reuptake inhibitors (SSRIs) in particular, such as citalopram, sertraline and escitalopram, are associated with accelerated cognitive decline. Patients taking these drugs lose their mental abilities more quickly and have a higher risk of severe dementia. In addition, higher doses are associated with an increased risk of fractures and increased overall mortality.
The scientists therefore recommend choosing antidepressants very carefully and reviewing their use regularly.
Alternatives to antidepressants
Instead of relying on medication, there are effective natural methods to prevent or treat depression and cognitive decline.
1. orthomolecular medicine
This therapy relies on a targeted supply of vitamins, minerals and trace elements that are essential for brain function. Studies show that an adequate supply of vitamin D, B vitamins, omega-3 fatty acids and magnesium can alleviate depressive symptoms and promote cognitive health.
2. traditional Chinese medicine (TCM)
TCM methods such as acupuncture, herbal medicine and Qi Gong help to stabilize emotional balance and have been shown to reduce stress and depression.
3. neurofeedback – the revolution in brain research
Neurofeedback is one of the most promising non-drug methods for treating depression and dementia. This method works by specifically training brain waves to bring brain activity into a healthy state.
📌 Advantages of neurofeedback:
✅ Reduces depressive symptoms threefold compared to conventional methods.
✅ Delays cognitive decline in dementia patients.
✅ Can improve cognitive function in some cases.
✅ Strengthens motor skills and spatial awareness to prevent falls.
Neurofeedback starts where medication often fails – it actively improves the self-regulation of the brain and thus offers a sustainable solution without side effects.
Summary of the study
A Swedish long-term cohort study (Mo et al., 2025) with 18,740 dementia patients investigated the relationship between antidepressants, cognitive decline and health risks. The most important results:
| Drug | Annual deterioration in cognition (MMSE points) | Increased risk of fractures and mortality |
|---|---|---|
| Citalopram (SSRI) | -0,41 | Yes |
| Sertraline (SSRI) | -0,25 | Yes |
| Escitalopram (SSRI) | -0,76 | Yes |
| Mirtazapine (other) | -0,19 | Yes |
| Amitriptyline (TZA) | No significant deterioration | No |
🔍 Higher doses of SSRIs led to faster cognitive decline and increased health risks.
🔍 The researchers recommend that antidepressants should only be used with caution and that regular checks should be carried out.
Conclusion: opt for natural alternatives!
This study shows that antidepressants are not the best choice for older people with depression or dementia. Natural methods such as orthomolecular medicine, TCM and above all neurofeedback offer a sustainable solution without side effects.
📌 My personal advice:
👉 Avoid antidepressants if there are alternatives!
👉 Rely on neurofeedback – a highly effective, scientifically proven method.
👉 Support your mental health with targeted nutrition and natural healing methods.
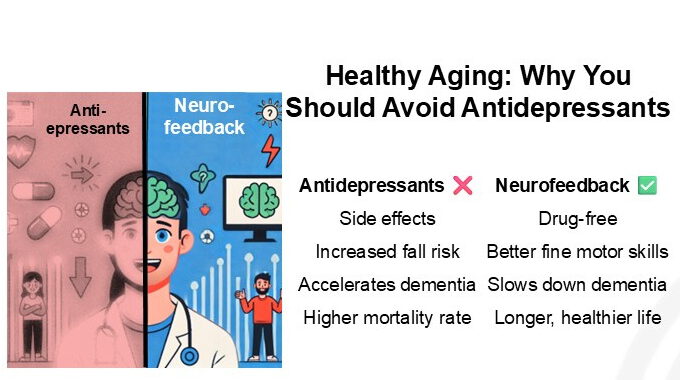
| Antidepressants ❌ | Neurofeedback ✅ |
|---|
| ❌ Side effects: Fatigue, weight gain, dependence | ✅ Without medication: no chemical stress for the body |
| ❌ Increased risk of falling: weakens motor skills & balance | ✅ Better fine motor skills: strengthens coordination & body control |
| ❌ Accelerates dementia: Increases cognitive decline | ✅ Slows down dementia: promotes brain plasticity & memory |
| ❌ Increased mortality: higher risk of fractures & diseases | ✅ Live healthier for longer: Supports the brain & nervous system |
If you would like to find out more about neurofeedback and natural forms of therapy, please let me know! 😊
Summary of the study “Antidepressant Use and Cognitive Decline in Patients with Dementia: A National Cohort Study”
Authors: Minjia Mo et al. (2025)
Source: BMC Medicine, DOI: 10.1186/s12916-025-03851-3
Study period: 2007-2018
Data source: Swedish Register for Cognitive and Dementia Disorders (SveDem)
Study structure and methodology
Study design
- Type: National cohort study
- Location: Sweden
- Inclusion criteria: Patients with newly diagnosed dementia, recorded in SveDem
- Observation period: From the time of diagnosis until October 16, 2018
- Sample: 18,740 patients (54.5 % women, average age 78.2 years)
Measurements
- Main variable: Antidepressant use (defined as at least one prescription)
- Assessment of cognitive decline: Mini-Mental State Examination (MMSE)
- Primary outcome: Cognitive change over time
- Secondary outcomes:
- Severe dementia (MMSE < 10)
- Fractures
- Mortality
- Statistical analyses:
- Linear mixed models for analyzing the MMSE progression
- Cox proportional hazard models for calculating the risk of dementia deterioration, fractures and death
Results
Antidepressant use in the cohort
- Number of patients on antidepressants: 4,271 (22.8 %)
- Most common class: Selective serotonin reuptake inhibitors (SSRIs) (64.8 %)
- Most commonly used medication:
- Citalopram (SSRI)
- Mirtazapine (other antidepressants)
- Sertraline (SSRI)
- Escitalopram (SSRI)
- Amitriptyline (TZA)
- Venlafaxine (SNRI)
Influence on cognitive changes
| Drug | β-value (annual change in MMSE points) | Significance |
|---|---|---|
| All antidepressants | -0,30 | p < 0,001 |
| Sertraline (SSRI) | -0,25 | p = 0,011 |
| Citalopram (SSRI) | -0,41 | p < 0,001 |
| Escitalopram (SSRI) | -0,76 | p < 0,001 |
| Mirtazapine (other) | -0,19 | p = 0,014 |
- Patients on antidepressants showed faster cognitive deterioration than non-users.
- The strongest negative effect was observed for escitalopram (-0.76 MMSE points per year).
- The effect was particularly strong in patients with severe dementia (MMSE 0-9).
Influence on other health risks
| Outcome | Hazard Ratio (HR) | Significance |
|---|---|---|
| Severe dementia (MMSE < 10) | 1,35 | p = 0,035 |
| Fracture risk | 1,18 | p < 0,001 |
| Mortality (all causes) | 1,07 | p = 0,016 |
- Higher SSRI doses were associated with an increased risk of severe dementia, fractures and death.
Dose-response relationship
| Dose range (DDD = defined daily dose) | β-value (annual change in MMSE points) |
|---|---|
| ≤ 0.5 DDD | -0,20 |
| > 0.5 / ≤ 1.0 DDD | -0,33 |
| > 1.0 DDD | -0,37 |
- Higher doses of SSRIs led to greater cognitive decline.
Conclusions
- Antidepressants accelerate cognitive decline in dementia patients.
- SSRIs (especially escitalopram) have the strongest negative effects.
- Higher SSRI doses increase the risk of severe dementia, fractures and mortality.
- Regular monitoring of antidepressant use in dementia patients is necessary.
This study underlines the need for cautious and individualized use of antidepressants in patients with dementia, as their benefit may be questionable and the risk may be high.
Mo, M., Abzhandadze, T., Hoang, M. T., Sacuiu, S., Grau Jurado, P., Pereira, J. B., Naia, L., Kele, J., Maioli, S., Xu, H., Eriksdotter, M., & Garcia-Ptacek, S. (2025). Antidepressant use and cognitive decline in patients with dementia: a national cohort study. BMC Medicine, 23(82). https://doi.org/10.1186/s12916-025-03851-3
Terms and abbreviations
p-value (p-value)
The p-value indicates how likely it is that a certain result occurred by chance.
- Small p-value (e.g. p < 0.05) → The result is statistically significant. It is very unlikely that it was only due to chance.
- Large p-value (e.g. p > 0.05) → The result is not significant, it could have arisen by chance.
Example: If there is a p-value of 0.001, this means that the probability that the result is just chance is 0.1%.
β-value (beta coefficient)
The β value shows how strongly one variable influences another.
- Negative β-value → The variable causes a decrease.
- Positive β-value → The variable causes an increase.
Example:
- β = -0.30 for antidepressants means that patients taking antidepressants lose 0.30 points per year faster on the MMSE scale (Mini-Mental Status Test) than patients not taking antidepressants.
The greater the magnitude of the β value, the stronger the effect.
DD (Defined Daily Dose, DDD = Defined Daily Dose)
- The DDD is the amount of a drug that an average adult needs daily to achieve a normal effect.
- This unit of measurement helps to make different drugs comparable.
Example:
- 1.0 DDD means that a patient takes exactly the recommended daily dose.
- >1.0 DDD means a higher than recommended dose, which is often associated with more severe side effects.
SSRIs (selective serotonin reuptake inhibitors)
SSRIs are a group of antidepressants that are often prescribed for depression and anxiety disorders.
- They increase the serotonin level in the brain, a “happiness hormone” that stabilizes the mood.
- Well-known SSRIs are citalopram, sertraline and escitalopram.
According to the study, SSRIs are associated with faster cognitive decline in dementia patients.
Hazard ratio (HR, risk ratio)
The hazard ratio (HR) shows how much an event (e.g. death or fracture) changes in one group compared to another group.
- HR = 1 → No difference between the groups.
- HR > 1 → Higher risk for the event.
- HR < 1 → Lower risk for the event.
Example:
- HR = 1.18 for fractures means that people taking antidepressants have an 18% higher risk of fractures than people not taking antidepressants.
- HR = 1.35 for severe dementia means that the risk of severe dementia is increased by 35%.
Summary for laypersons
- p-value: Shows whether the result is random. A value below 0.05 means that it is very likely a real effect.
- β-value: Shows how much a medication changes something. Negative values mean a deterioration, e.g. faster memory loss.
- DDD: A standard dose indication for drugs to make different doses comparable.
- SSRI: A type of antidepressant that is often used but was associated with faster cognitive decline in the study.
- Hazard ratio: Shows how much a risk increases or decreases. Values above 1 mean a higher risk of a certain event (e.g. death or fractures).